By Byrhonda Lyons and Jocelyn Wiener, CalMatters
On the last day of Adam Collier’s life, he had breakfast in his cell in Kern Valley State Prison. He wrote two letters, one to his mother, the other to the guard who would later find his body.
During the previous four years in prison, Collier had been hospitalized for mental health crises 14 times. His many letters to family and friends wobbled between lucidity and gibberish. His medical records proffered graphic descriptions of self-harm. Collier had originally landed in prison for exposing himself to women in public while high on meth. Ashamed and delusional, he tried to castrate himself with a broken plastic cup because he believed it was God’s desire.
The prison system’s response to Collier’s increasing anguish?
Transfers.
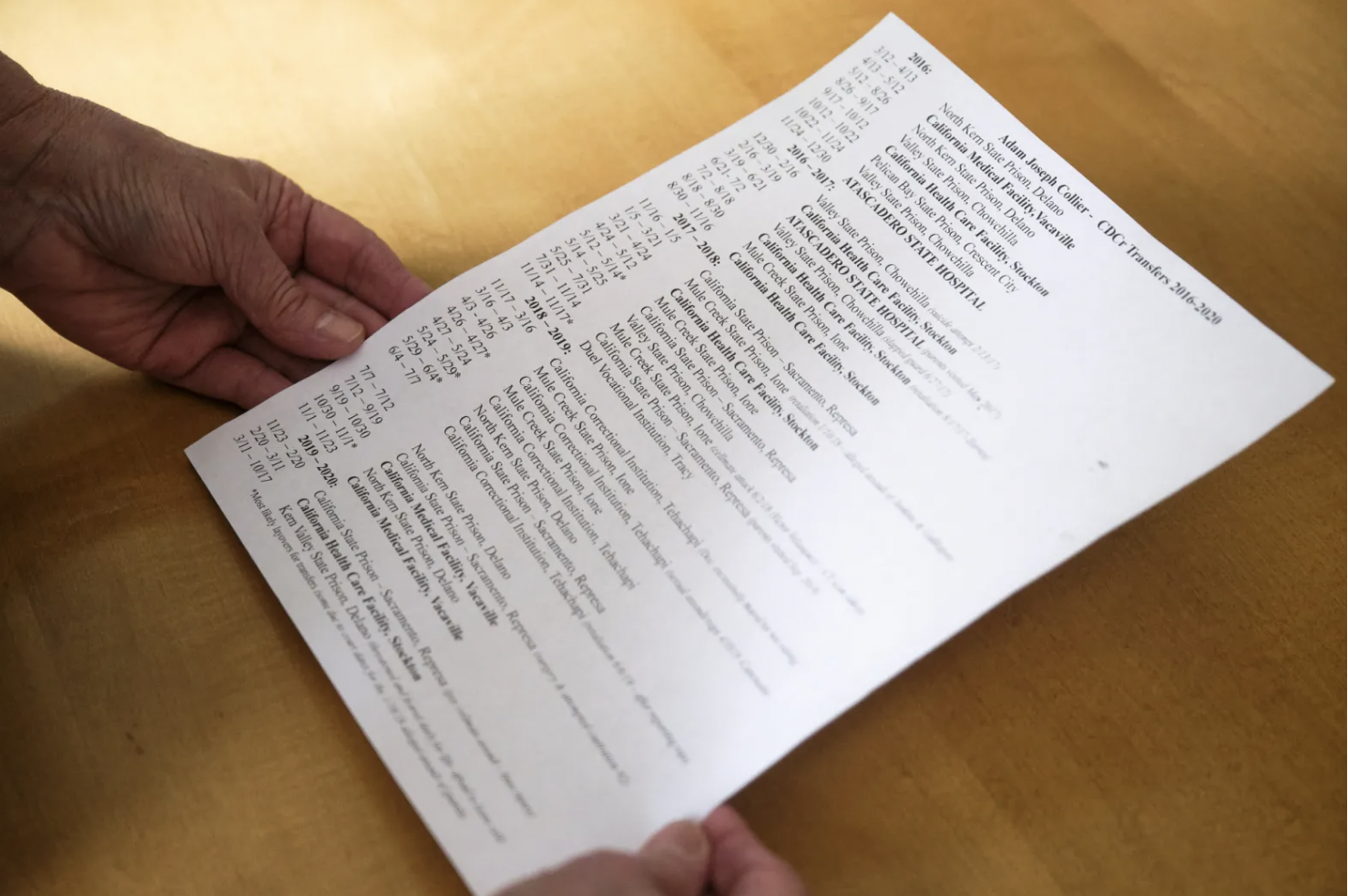
Between 2016 and 2020, the California Department of Corrections and Rehabilitation transferred Collier 39 times, ping-ponging him between mental health crisis beds and increasingly high security prisons at a pace so fast he told his mother, Susan Ottele: “I’m fucking dizzy.”
On Oct. 17, 2020, at age 43, he killed himself.
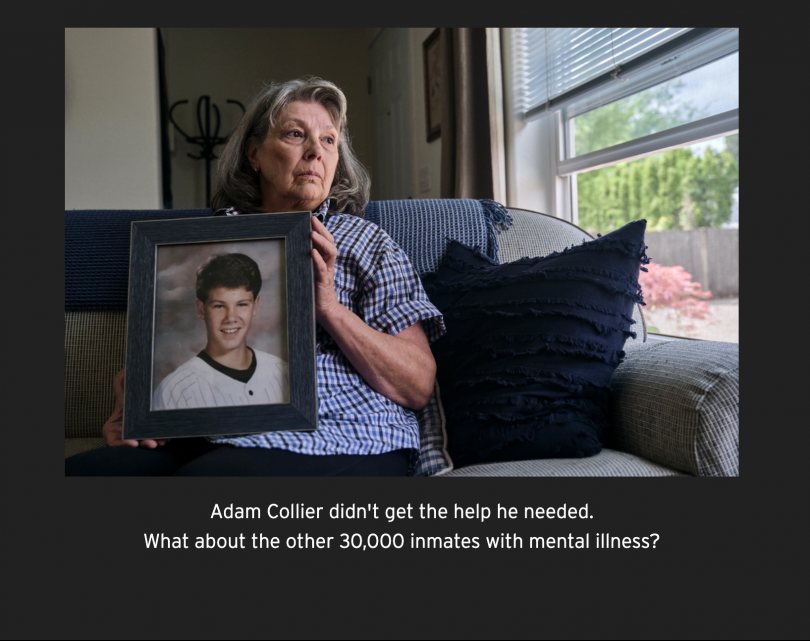
Three decades after California’s prisons first came under court monitoring for rampant abuse and neglect of prisoners with mental illness, the system is still failing to protect its sickest inmates. For many of these men (the vast majority of people behind bars are male) prison is not a place to heal. It is a place to disappear.
The constant relocation that Collier experienced is a symptom of the system’s brokenness. Too often, in lieu of an effective treatment plan, challenging inmates are simply moved along, a CalMatters investigation has found.
After Collier’s death, state overseers found the department had “poorly handled” his case. The Office of the Inspector General, which provides independent oversight of prisons, described an array of internal problems, including clinicians improperly delaying Collier’s referral to a higher level of care and failing to adequately document his history of self-harm. Earlier this year, his parents filed a wrongful death complaint in federal court.
The California Department of Corrections and Rehabilitation failed to respond to several requests by CalMatters for an interview but sent written answers to emailed questions. Department representatives declined to comment on Collier’s case, citing health privacy laws.
Corrections spokesperson Vicky Waters said the department, along with California Correctional Health Care Services — which are jointly responsible for medical services to the state’s prison inmates – provide “quality medical and mental health care.”
“Much like it works in a community health care setting, individuals may need to physically move to the appropriate facilities to receive the necessary level of care,” Waters said.
Several attorneys and researchers steeped in advocacy for this population said they were stunned by the speed at which Collier was shuffled around the system. Some told CalMatters they initially didn’t believe it until they saw the documentation.
“I don’t think the system is designed where anybody says, ‘Stop. Take a step back. What does he really need?’” said Margot Mendelson, an attorney with the Prison Law Office, co-counsel in the ongoing federal, class-action suit about the state’s treatment of inmates with mental illness, known as Coleman.
For many inmates, the churn continues.
The Department of Corrections and Rehabilitation agreed on May 5 to release transfer data that CalMatters had requested in March, but has thus far failed to provide it. However, data collected by CalMatters from the department’s public website between June 2021 and May 2022 showed that, while most of the state’s prison inmates rarely move, a subset is being transferred frequently. According to CalMatters’ analysis of the data, of the 86,118 inmates who had been incarcerated at least 12 months prior to last June, 1,988 moved at least four times this past year and 32 moved eight times or more. Several of the inmates who moved the most frequently told CalMatters they were being treated for mental health conditions.
Even as the state shrunk its overall prison population in recent decades, the ranks of inmates with mental illness continue to swell. In April 2000, one in eight California prison inmates had a diagnosed mental illness. This year, one in three do, according to data provided by attorneys from San Francisco-based Rosen, Bien, Galvan & Grunfeld, which is co-counsel in the Coleman suit.
Long before he arrived at Kern Valley State Prison in March of 2020, Collier was diagnosed with post-traumatic stress disorder, bipolar disorder, borderline personality disorder and anxiety disorder, among others. He had spent five years in Oregon State Hospital and several months in a California state hospital.
Prisoners’ rights advocates have long argued that prison is not the right setting for people with serious mental illnesses. For the many who wind up behind bars anyway, Collier’s story poses a critical question: Are frequent transfers a good solution for anyone?
A sensitive child suffers trauma
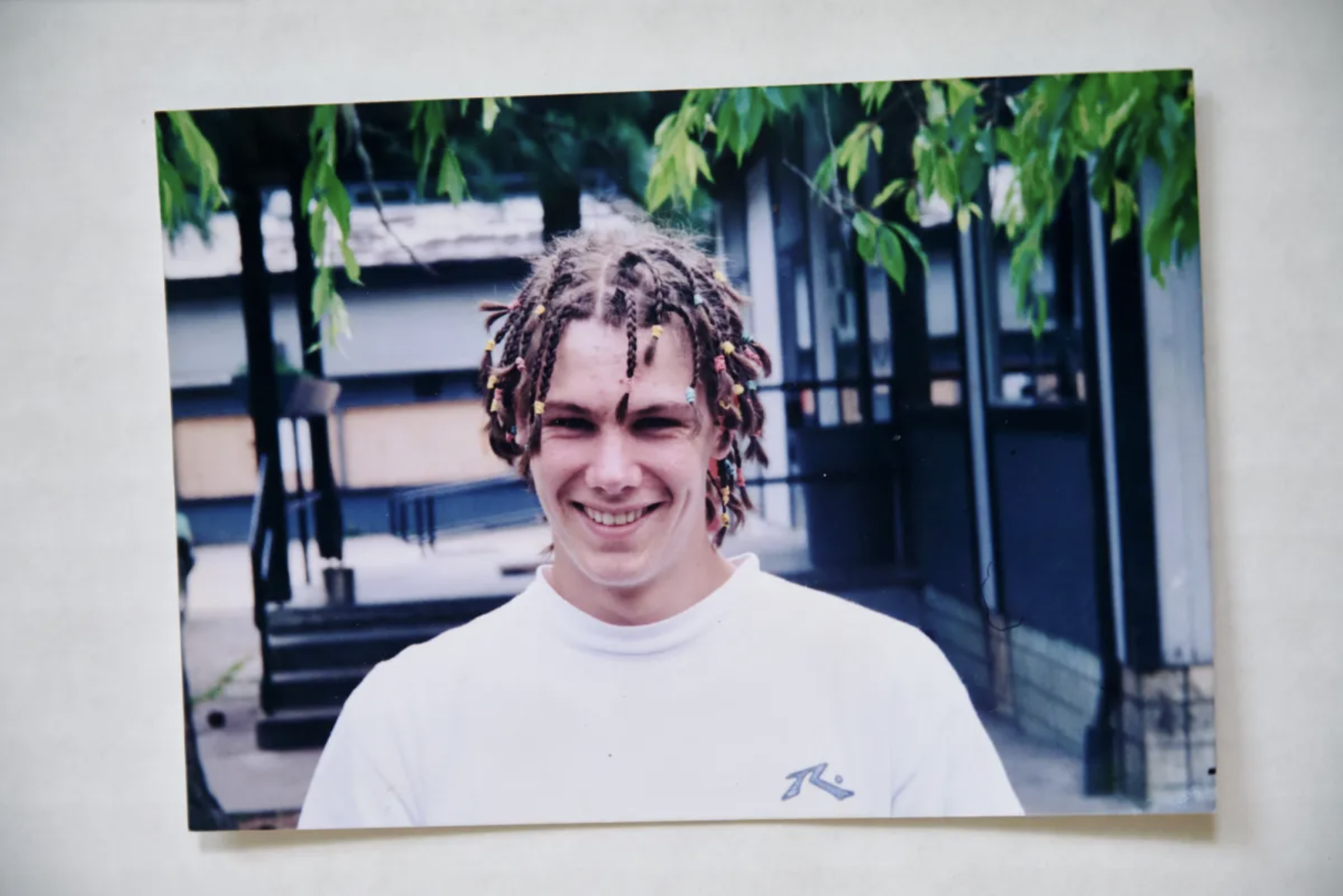
As a child, Collier was sweet-natured and sensitive, a tow-headed boy who made friends easily and loved teddy bears, chess and snuggling with his dog, Jessica, his mother recalled. In his first five years, his family lived off the grid in the mountains near Grants Pass, Oregon. After moving to Santa Cruz for a time, his parents divorced when he was 7. His mother moved Adam and his older brother back to the Portland suburbs.
Susan Ottele still has a note Adam carefully printed out for her in wobbly letters during that time: “How was work today? I missed you all day.” A few years later, he brought home a certificate from CF Tigard Elementary School, commending him for being kind-hearted.
In middle school, he met a crew of close friends, including his best friend, Anton Engelmann. After Engelmann shared his personal troubles with Collier, Engelmann recalled, Collier regularly brought him home for a meal and a shower.

Engelmann said he remembers watching Collier jump up to hug his mother whenever he saw her. But Susan Ottele was gone a lot, too. A single mom, she sometimes worked as many as 18 hours a day.
Left to their own devices, Collier and his friends would skip school to egg houses, set off illegal fireworks and smoke pot, Engelmann and other friends recalled.
Only much later did his friends and family discover the extent to which Collier had been living a nightmare during those early years. At various points, several different men abused him physically and sexually, according to his mother, friends and prison medical records.
That trauma tormented him for the rest of his life. He attempted to kill himself when he was 12 or 13, according to medical records obtained by his mother. He would try again at least seven more times.
As the years went by, Collier went on and off psychiatric medications, telling his mother he didn’t like the way they made him feel. He increasingly self-medicated with street drugs.
“The things that happened to him really hurt his head and his heart, and drugs was a good numbing effect and a good distraction, I guess,” said his former girlfriend, Rhapsodee Murray. “But I also think it broke his brain.”
In his early 20s, after a stint in jail, Collier met another girlfriend, Miki Cornilles, at a rehabilitation program on a working farm. Cornilles was drawn to his humor and kindness. They eventually moved into an apartment and began using drugs together, she said. Cornilles was troubled by how intensely meth affected Collier. One day, she recalled, his mother brought over a new set of dishes. Collier threw it in the garbage.
“I don’t need all that material shit,” he said.
Beginning in his 20s, Collier was arrested multiple times in Oregon for exposing himself, the same crime that would eventually land him in prison in California. In Oregon, Collier was found “guilty except for insanity” and sent to Oregon State Hospital for five years in February 2007.
While there, Collier underwent surgery to address chronic back pain. Something went wrong — the spinal screws snapped. From then on, according to medical records, Collier lived with intense pain, which compounded his stress. At one point, he pounded the wall of his room in the state hospital so hard he broke his hand.
In December 2011, Collier was discharged from the Oregon State Hospital. For a few months, he lived in his mother’s house in McMinnville, a quaint wine country town outside Portland. The next summer, Collier decided to move closer to his father’s family in Santa Cruz.
He was ready, he told his mother, to start over.
How the system works — or doesn’t
Why did Adam Collier transfer so often?
Advocates, inmates and family members contend that, in cases like his, a steady stream of transfers reflects a system that too often fails to adequately care for people in mental health crises. These inmates might bounce between prisons and short-term crisis beds without ever stabilizing enough to get better, they say. For some, the simple fact of being in a prison environment might trigger them to lash out against guards or other inmates.
Corrections spokesperson Waters said in a statement that inmates can be transferred for a variety of reasons, including court hearings, medical treatment, mental health treatment, changes in security level, patient safety, staff conflicts, misconduct allegations or parole.
Six of California’s 34 prisons don’t have mental health programs, she said, “so patients requiring ongoing mental health care would need to be transferred.”
Clinicians “are trained to identify and treat serious mental illness, and tailor care to the individual needs of patients,” Waters stated.
Mental health care in California’s prisons is provided along a spectrum, designed to transfer inmates as their level of need changes. Treatments range from outpatient therapy in the general inmate population to long-term hospitalization in dedicated treatment facilities within the correctional system.
At the other end of the spectrum are state hospitals, which are separate facilities that also house people who are not in the criminal justice system.
Suicidal inmates are supposed to be moved quickly to mental health crisis beds, according to the state’s mental health program guide. The beds are designed for a 10-day stay that can only be extended by medical officials.
But the system doesn’t always work perfectly. Sometimes people who need it aren’t referred to a higher level of care, the Inspector General has determined in several investigations.
Sometimes referrals come too late.
In 2019, mental health clinicians failed to evaluate acute suicidal risk factors in one inmate after he learned of his mother’s death. They didn’t place him under suicide watch or send him to a mental health crisis bed, according to a report from the Inspector General. Soon after, he killed himself.
Adding to these concerns, the state and country face a shortage of mental health providers, which experts say has only worsened during the pandemic.
Waters said in an email that the department has robust recruitment and retention programs, which she calls “especially critical.”
She said the department routinely assesses the number of mental health crisis beds and inpatient beds to make sure it has enough to meet fluctuating needs.
But some say a provider and bed shortage means inmates don’t always get the mental health care they need.
“The idea is, ‘How soon can we stabilize them and get them out?’” said Keramet Reiter, a criminology professor at the University of California, Irvine.
When inmates repeatedly get into mental health crises and act out or hurt themselves, correctional officers and even prison clinicians often view those actions as manipulative, Reiter and others said. These inmates can then be deemed more dangerous and moved to higher security facilities where people with mental illness are even more vulnerable.
Those who are classified as sex offenders, as Collier was due to his indecent exposure charges, have it worst.
Even if inmates are extremely sick, state hospitals are often wary of admitting those with high security levels or histories of bad behavior, said Jessica Winter, an attorney with the Rosen, Bien, Galvan & Grunfeld.
Her firm is co-counsel for Coleman, the federal class-action suit on behalf of inmates with serious mental illness. That case has led to important reforms, she and other advocates say, including more oversight of how California’s prisons treat inmates with mental illness than exists in some other states.
In theory, transfers can mean the system is working, said Tom Nolan, another attorney at Rosen, Bien, Galvan & Grunfeld.
But in Collier’s case, he said: “It’s kind of crazy how much he got transferred around.”
Collier’s start-over plan disintegrates
Adam Collier’s plan to start over in Santa Cruz was short-lived. It was 2012, and he was 35 years old when he left Oregon for California.
During his first year and a half in Santa Cruz, he was arrested several times for indecent exposure. Under Jessica’s Law, he was required to register as a sex offender and was barred from living many places. He cycled between homeless shelters, the streets and jail.
A psychologist who evaluated Collier around that time considered him incompetent to stand trial, saying he was agitated, heard voices, needed medication, and was asking for treatment, according to court records reviewed by CalMatters.
On April 29, 2013, Santa Cruz police picked him up for exposing himself in a public place. Collier took a plea deal and was sentenced to two years in prison.
Collier served time in San Quentin and was released. His mother looked into bringing him back to Oregon to serve his parole, but said her county wouldn’t allow it. She couldn’t afford the move to California, though she said she contemplated coming anyway and living in her car.
Within weeks, he was arrested again in Monterey and sent to jail.
The next year, the cycle repeated. But this time, he was sentenced to five years in prison.
That’s when Susan Ottele started tracking her son’s movements.
On March 12, 2016, according to her notes, Adam Collier arrived at North Kern State Prison.
His first transfer, to California Medical Facility in Vacaville, took place a month later.
His second, back to North Kern, was the month after that.
Reiter of UC Irvine calls what happened to Collier — bouncing between crisis units and state hospitals and seven different prisons— “a very sad and very unsurprising story.”
There’s even a term for it, she said: “Diesel therapy” refers to moving challenging inmates around to keep them from wearing out staff in any given facility.
“It absolutely happens often,” she said.
In a February 2017 letter to his mother, Adam Collier said he believed he was sometimes moved as punishment for his behavior.
Collier did lash out at prison staff, sometimes dangerously. CalMatters’ review of nearly 600 pages of his prison medical records from 2020, shared by his mother, shows he was written up multiple times for spitting, fighting and battery against prison staff.
At one point, he was moved to segregated housing after attacking several prison guards.
“You are deemed a threat to the safety and security of this institution, its staff and inmates,” wrote the prison lieutenant who authorized that move.
Such circumstances can be taxing for all involved.
“Staff work in the same conditions that incarcerated people live in,” said Margot Mendelson of the Prison Law Office. “Really toxic environments are toxic for everyone.”
Inmates describe multiple transfers
For a year, CalMatters monitored the statistical evidence of thousands of people being shuffled around the prison system. Without state data, as CalMatters requested, the full extent of these relocations over time is unknown.
Several inmates who moved at least five times in the last year told CalMatters the constant transfers prevented them from establishing relationships with therapists. With every transfer, they said, they often lost their few possessions. They were shocked that someone outside the system even noticed.
“It makes my mental health worse,” said Steven Saucedo, 48, who has transferred at least eight times since last June, including relocations to attend court, CalMatters data shows. “You’re always on the move.”
Cedrick Johnson, 61, said he didn’t start moving until he was diagnosed with schizophrenia a few decades ago. He’s been incarcerated since the 1980s.
“(Transfers) are a great problem,” he said, sighing. “We talk to different doctors all the time. … It doesn’t make you better at all.”
Johnson said he has transferred at least seven or eight times since last June; CalMatters has documented eight moves to five facilities in less than a year.
Randall Shrout, an Amador County public defender who represented Collier in a 2018 case, said frequent transfers are common among his clients, many of whom come through Mule Creek State Prison in Ione.
“You’ve got Adam’s name, and there are hundreds of others,” he said. “I can go through 10 years of records and find you mental health cases where they bounced them all over the state.”
Jennifer Hoff, whose 29-year-old son has suffered from serious mental illness since he was a young child, said he has been in at least nine different prisons, and has transferred numerous times in the past decade.
“It’s meant to grind you to dust,” she said.
Her son, Matthew, has schizophrenia. He was charged with terrorism in 2012 at age 19, his mother said, after he walked, unarmed and off his medication, into a bank and passed a sticky note to the teller threatening to blow himself up if they didn’t give him $1,000.
In prison, he has repeatedly harmed himself, including carving up his face with a needle, she said. Some years he has been transferred between facilities nearly a dozen times, she said. Each time requires him — and his family — to start over with new staff and new routines.
“You can’t possibly keep up with the transfers,” she said. “How engaged can you possibly be in a system that’s meant to make you go away completely?”
‘I guess this is my lot’
Every day for four years, Susan Ottele would log onto her computer to check on her son’s whereabouts.
She kept a list of the various prisons’ phone numbers. Every time he moved, she called all the numbers on the new facility’s phone tree until she knew how to reach someone if something went wrong.
Something always went wrong.
She felt a growing sense of helplessness.
“It’s like being strapped to a chair watching your child being tortured,” she said. “Once you get in the prison system, there isn’t much you can do.”

Collier wrote to his mother, often complaining about back pain that drove him to tears.
“I guess this is my lot,” he wrote from North Kern State Prison in May 2016. “See why heroin and vodka seems appealing?”
At times, he sprinkled in words of reassurance, along with updates on his sobriety:
“Please don’t worry about me.” “I’m not suicidal.”
Trying to get him help, Susan Ottele penned certified letters in loopy cursive begging prison wardens to give her son Tylenol and heating pads.
“Adam’s pain management is crucial to his mental + physical health,” she wrote. “Allowing him to suffer needlessly is neglectful and a form of torture to say the least.”
In February 2017, Adam Collier attempted suicide again. He was sent to California Health Care Facility, Stockton and then to Atascadero State Hospital for three months. He did well there, his mother said, but was returned to Valley State Prison in Chowchilla in late June. From there, things unraveled.
With a parole hearing approaching, he told his mother he was afraid of being sent back out to live on the streets. He slapped a prison guard.
He was transferred again. And again. And again.
The following year, in January 2018, he was accused of threatening and kicking a prison guard at Mule Creek State Prison, and was ordered into solitary confinement.
In an appeal, Collier wrote that multiple guards had handcuffed him and beaten him until he was unconscious. Susan Ottele wrote to the warden, who replied that the staff’s actions were in compliance with the department’s use of force policy.
Oversight weak, documentation ‘lax’
Susan Ottele filed several complaints with the independent Office of the Inspector General about Collier’s medical care at Mule Creek and the alleged use of force.
The oversight body is known for scathing public reports about prison misconduct. That’s about all it can do. In 2011, lawmakers stripped the office of its authority to investigate prison employee misconduct, effectively leaving the Department of Corrections and Rehabilitation to police itself. Last year, legislative staff recommended the inspector general’s authority be reinstated. It wasn’t.
CalMatters analyzed 372 critical incident case summaries from the office since 2018. Of 67 inmate suicides reviewed by the inspector general, 81% percent were determined to be “poorly” handled by the state. Among those suicides, CalMatters identified 38 where the office dinged state mental health professionals for not referring inmates to a higher level of care, keeping lax documentation or returning people to their housing units despite increased mental health symptoms, among other things.
Over the years, Adam Collier’s letters were often punctuated with allegations of brutality and victimization: a cellmate he said knocked him unconscious, prison guards sodomizing him with a baton. His medical records, meanwhile, describe him acting out against guards, spitting at them or hitting them with his cane.
For a while, he went on a hunger strike.
During his time in prison, Collier was prescribed at least 19 different psychiatric medications. He would take them for a while, his mother said, then stop due to the side effects.
By 2019, he began sending her long screeds praying for plagues to rain down on the United States, along with lists of elaborate burial wishes: the broken screws in his back should be removed upon his cremation and placed in the parking lot of the Oregon State Hospital; his ashes should be scattered in Santa Cruz Harbor at 4:30 a.m.

His medical records describe him cutting himself in order to “burn my blood for my God.” The records also mention him asking for more consistent mental health treatment.
That July, he again attempted to kill himself. A month later, he tried to castrate himself. He begged his mother to help him get mental health care.
“I believe good ol’ ‘Job’ did his best,” he wrote in one letter, referring to the Biblical character who is tormented to test his faith in God. “Patience hath an end.”
“Feed kitties treats 4 me,” he added.
COVID slips into the prisons
On March 11, 2020, according to his mother’s notes, Adam Collier transferred one last time.
Kern Valley State Prison, a maximum-security facility 40 miles northwest of Bakersfield, is one of six prisons named in a motion in a federal class action lawsuit alleging correctional officer abuse of people with disabilities. In a 2020 report to the Legislature, it was listed as having among the highest annual average suicides, due to being a high security facility that houses and treats inmates with severe and chronic mental health and behavior problems.
Inmates there, said Margot Mendelson, of the Prison Law Office, “live in terror.”
Around the time of Collier’s arrival, the country’s first COVID cases were popping up in Northern California. Soon, with prisons buckling under massive outbreaks, Gov. Gavin Newsom issued an executive order temporarily halting transfers.
Collier hated it at Kern Valley. During those first months of the pandemic, he described to his mother how isolated and depressed he felt, too terrified of prison guards and other inmates to leave his cell.
On one piece of lined paper, he scrawled a single sentence: “I loosing it mom.”
He was 43 years old then, and walking with a cane. His body was etched with scars from various attempts to kill himself.
On May 22, 2020, he tried again.
A week later, he told the psychologist who interviewed him that he had done so because he was high on meth and afraid of retribution for an unpaid drug debt, his medical records show. He asked to be sent to a state hospital or into solitary confinement for his own protection until he was eligible for parole the next January. The psychologist noted a history of “exaggerated, staged behaviors to manipulate CDCR staff to promptly respond” and that she deemed “intentional to drive/control the responses of others.” She also noted an increased risk of future self-harming events.
“…if you send me back, I’ll just keep doing this stuff,” the psychologist’s notes quoted Collier as saying. “I don’t want to die. I want to parole and never come back to prison. I want a cat, a surf board, a truck, a life, and now that Vegas is back open, strippers and to see my mom and dad.”
Friends who spoke to him during that time detected something wrong.
“When I first met him, he was just this bright shining light, and it was barely a dull lightbulb by the end,” said his former girlfriend, Rhapsodee Murray.
In July 2020, Collier wrote a letter to his mother describing a tiny cricket that wandered into his prison cell. He named it Jiminy, and talked about feeding it crumbs of graham crackers and pretzels. He liked to balance it in his hand and watch it sing.
“Out of 100 cells,” he marveled, “he chose mine.”
He was desperate, he told his mother, for a hug.
Susan Ottele says she called the prison 13 times that year, begging for help.
She and her son both held out hope that he would get transferred to a state hospital soon.
But Collier did not meet the “emergency transfer criteria” in place during COVID-19, according to a report on his suicide by a court-appointed expert. Instead, he stayed in his cell, getting sicker.
In October 2020, he refused 22 group treatment sessions, the report stated.
“You’re like my 30th clinician this term; love the continuity of care in CDCR,” Collier reportedly told one therapist.
On October 17, 2020, Collier was given breakfast in his cell, according to the federal lawsuit filed by his parents. He didn’t show up for lunch. Despite his documented history of self-injury and suicide attempts, no one checked on him for eight or nine hours, the complaint said.
At 3:32 p.m., a prison guard found his body.
An hour later, the phone rang inside Susan Ottele’s home.
The dreaded phone call
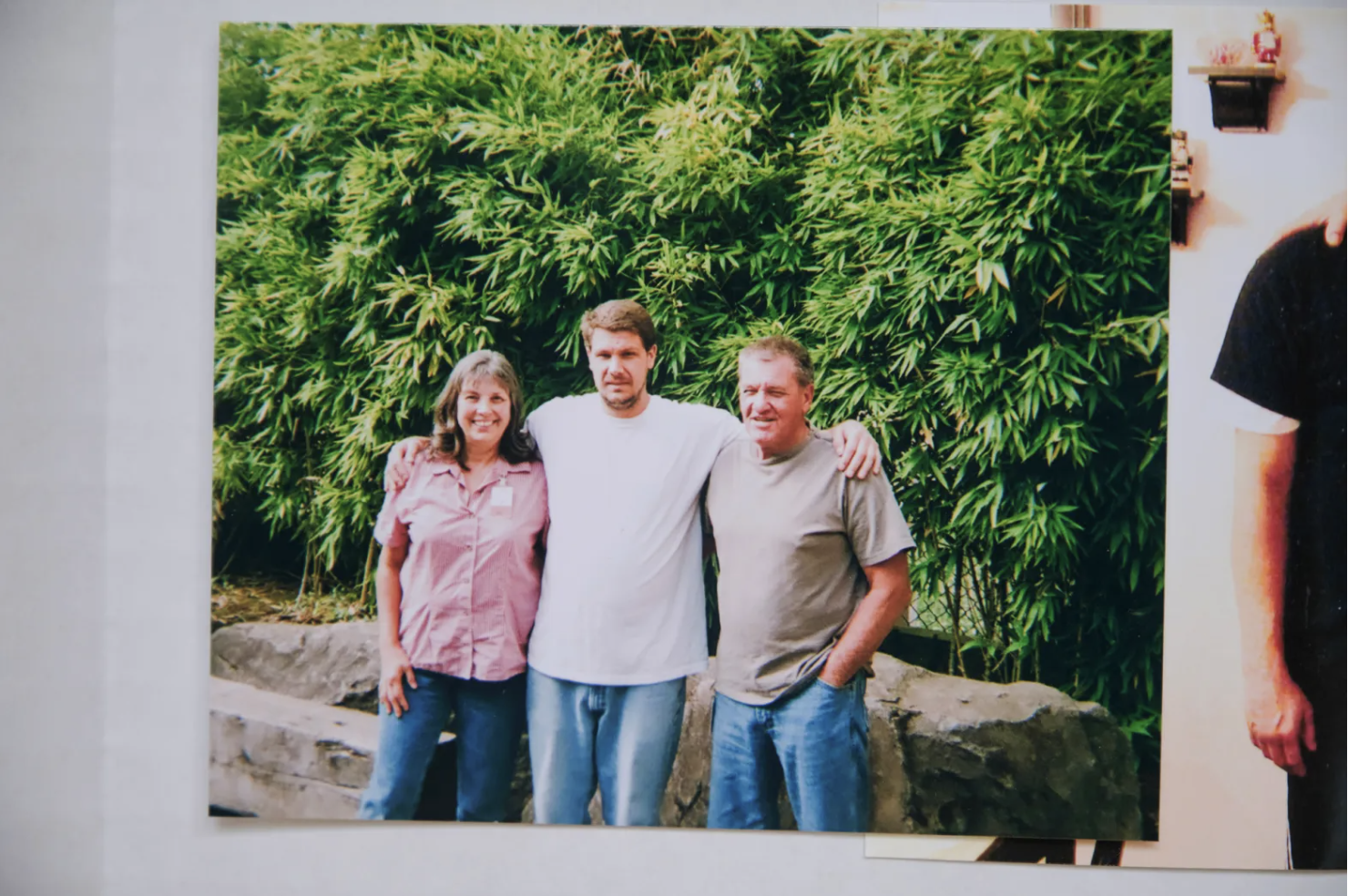
On a rainy day this spring, Susan Ottele sat in the living room of her neat beige and white prefabricated home in McMinnville, Oregon. The property is dotted with dogwood, fir, oak, maple and cedar. A series of bird feeders is visible out the back window.
A year and a half has gone by since she answered the phone, then collapsed to the ground, screaming.
Two weeks after her son’s death, Susan Ottele climbed into her 20-year-old GMC and drove 15 hours to Bakersfield to view his body and begin her search for answers to an unbearable question: Why did he die?
She has accumulated a collection of clues that, to her, point to institutional indifference: the fat metal spinal screws that were returned to her, snapped in half, after her son’s body was cremated. A binder full of his letters and her scrupulous documentation.
“He was crying out in pain,” she said. “The louder he got, the less they heard.”
His ashes sit on the dining room table in a blue velvet box, waiting to be scattered in the Santa Cruz Harbor. She keeps a collage of photos from his memorial service in the living room; as long as they’re up, she feels like he’s still with her.
Other people have also tried to unravel any missteps that might have contributed to Collier’s death.
In its review of his suicide, the Office of the Inspector General found that the prison department “….failed to adequately document self harm incidents, failed to provide proper risk ratings, and failed to follow procedure for referral to a mental health crisis bed.”
A Special Master appointed bythe court to investigate inmate suicides under Colemanfound that providers had underestimated Collier’s mental illness and failed to look at his case as a whole “which should have created a sense of urgency as he spiraled into hopelessness and psychosis.” Collier’s death, the expert’s report said, might have been preventable had he “received an appropriate level of care and adequate treatment.”
Six months after Adam died, a box was delivered to Susan Ottele’s front door.
Inside was almost everything her son left behind. Stained sweatpants. Long johns. Holey socks. A plastic bottle of instant Folgers coffee. The white plastic cup he drank it from. A bottle of cinnamon. Another of garlic salt. A volume of inspirational sayings that she had sent to him, along with a dictionary, an explainer on bipolar disorder and a biography of Gandhi. The two final letters he’d written, the one to her still in a sealed envelope.
Also in the box: a piece of the instrument he’d used to take his life.
If you or someone you know is having thoughts of suicide, there is help available.
Call the National Suicide Prevention Lifeline 1-800-273-8255 (TALK) for resources and support. Free, confidential, available 24/7.
Text “HOME” to the Crisis Text Line—741-741—to reach a trained crisis counselor. Free, confidential, available 24/7.
For more information and resources, visit: SpeakingOfSuicide.com/resources
This article was originally published by CalMatters.
Data and graphics by Jeremia Kimelman and Erica Yee. Feature photo of Susan Ottele by Tojo Andrianarivo. Video byByrhonda Lyons. Animations by Crystal Tai. Production by Liliana Michelena.

What are the difficulties in dealing with mentally sick inmates? I used to work inside the jail and watched the inmates’ brutality. In some respects, I felt like I was developing despair and anxiety. I have a strong sense that something is wrong with me. I spoke with a doctor from https://www.therapysummit.com/, and they recommended that I undertake various therapies. I did, and after many sessions, I felt a lot better psychologically.